NEW YORK — Many people hope for a good death, even plan for it, but few prepare for it as thoroughly and cheerfully as Shatzi Weisberger. She had a certificate in the Art of Dying from the Open Center in New York City, and she helped run a monthly discussion group on the subject in Brooklyn, and another one in her small Manhattan apartment.
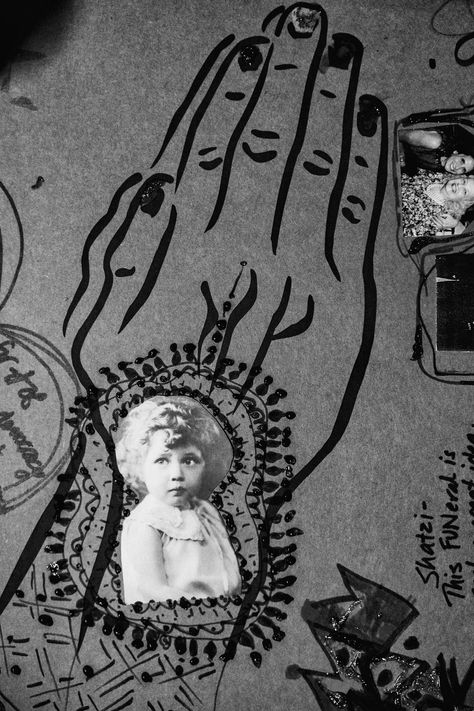
In June 2018, she held a FUN-eral for herself, where friends decorated a full-size cardboard casket, writing messages such as “Go Shatzi! (but not literally).” She wore a bright floral-print blouse for the occasion.
“I really want to experience my dying,” she said at the FUN-eral. “I don’t want to die in a car crash or be unconscious. I want to be home, I want to be in my bed, I want to share the experience with anybody who’s interested.”
Then this October, at age 92, Weisberger received a diagnosis of pancreatic cancer, untreatable. In mid-November she called from the hospital to invite The New York Times to follow her in this last stretch of life.
“I got my wish,” she said on that first phone call, on Nov. 18. “I did not want to die suddenly. I wanted to experience the dying process. And I am experiencing it. I’ve had some amazing experiences, absolutely incredible.”
Did she want the reporter to bring her a cannabis edible?
She did.
She was part of what has been called the “positive death movement,” a loose umbrella of Death Cafes, academic programs, books, YouTube videos and lectures that emerged in the past two decades, all aimed at dispelling fear and silence around death.
She had spent years studying death as an abstraction, urging others to approach it with joy and wonder. Now, she faced a cancer that is relentlessly concrete, and a health care system that is both fractured and, since COVID-19, grievously understaffed.
Her oncologist gave her a month, she said, maybe two or three. In the end, she would have less than two weeks.
The plan
Years before her diagnosis, Weisberger prepared the script for her last days.
She had a burial plot, a funeral director, a shroud and instructions for how she wanted her body to be handled after she died. A friend from the Art of Dying class promised to stay with her whenever the end approached.
“She preselected certain people for certain roles,” said David Belmont, a friend whom she tapped to navigate the health care system.
She kept an ever-changing bequeathal list for her possessions, and stuck labels on everything showing who should get what.
She had been a nurse for 47 years, including caring for AIDS patients, so she knew her way around a deathbed. She was as ready as she could be.
At the hospital on Nov. 18, Weisberger talked about life after a terminal diagnosis. Now that her death was no longer a far-off hypothetical, was it living up to her expectations?
She was in tremendous pain, she said, and weakened from a sleepless night. But she was beaming, more at ease than I had ever seen her, even at her FUN-eral. Finally, all her years of work were coming to fruition. “I’m experiencing the best time of my life,” she said.
She shared what she called “a transcendental experience.”
A friend from Jewish Voice for Peace, an advocacy group that has been a passion in her life, had recently come to the hospital and massaged her back and feet. Weisberger had had massages before, she said, but this was a revelation.
All her life, she had recoiled from physical intimacy, she said, citing trauma in her childhood. But during her friend’s massage, she let down her guard. “For the first time, I allowed myself to be open to the intimacy,” she said. “And it was probably the most remarkable experience I’ve ever had.”
Through a friend, she made contact with her son, from whom she had been estranged for 50 years. Because she had never received nurturing from her parents, she said, she had not known how to give it to her children. “They deserved a whole lot better, he and his sister,” she said. She did not ask her son to forgive her, she said. “I hope that he can let go of any resentment, and realize, as I now do, that I did the best I could.” Her daughter rejected her attempt to reconnect.
Beyond these brief moments, though, having a terminal illness did not lead her to reassess her life. Instead, she talked about what was next, said Gina Colombatto, who stayed with Weisberger at the end.
“Instead of looking backwards, she had become excited about knowing: What is death?” said Colombatto, who, like Weisberger, calls herself a death educator. “The conflict was: But I still have things to do, and I don’t know what will death be like. I don’t know if I really want to go there, but I’m also excited, because I’m going there.”
The reality
Weisberger was determined to face death without painkillers. She believed that palliative care often meant a drug-induced stupor, leaving the patient too dazed to appreciate the experience of death. She wanted the full monty.
This was the first illusion she had to give up.
There were others.
After two weeks in the hospital, Weisberger wanted to return to her home for hospice care — a simple request, she thought. But Belmont was told that because of labor shortages, hospice organizations had two-week waiting lists.
Friends at Jewish Voice for Peace started a GoFundMe campaign to pay for private care — another step that Weisberger could not have taken for herself.
At home, her body was deteriorating faster than she expected. She could not move her legs to shift from bed to chair, and she could not remain in either for long without extreme pain. She ate little more than chocolate pudding, yogurt and apple sauce.
“I’m dealing with the disappointment of how fast my body is deteriorating, but I keep reminding myself, I can’t control it, so whatever happens, I’ll just deal with it,” Weisberger said.
The next day, Nov. 21, there were two documentary film crews in her tiny apartment. Vogue wanted to profile her. She wore a fentanyl patch and had a morphine elixir in case the pain got too severe, but so far, she was not using it.
She was in good spirits. “I’m not experiencing fear currently,” she said. “Certainly, it might happen. I think it probably will happen. I’m hoping I can transcend that. I’m very disappointed in the limited time I may have.”
I told her that I was leaving town after Thanksgiving, counting on her to hang on until I got back. Her last word to me was: “Enjoy.”
A good death?
The day after Thanksgiving, she had what she called a “pain emergency” and got the hospice doctor to increase her pain medication. For the first time, she sounded muddled on the telephone. Still, friends said she had good moments. Amy Cunningham, her funeral director, visited two days later and found her “glowing, with a ruddy look,” she said. “I left thinking it would be a January death.”
She noted Weisberger’s fastidious planning: a box along one wall, packed for the moment of death, was clearly labeled “SHROUD GOWN CANDLES,” with the names of the four women she assigned to wash and handle her body.
Three days later, on Wednesday, Nov. 30, Weisberger asked to postpone her interview with Vogue and told Colombatto that she did not want visitors. She increased her pain medication. She asked for the lights to be off. Whatever momentum had gotten her this far, Colombatto said, had given way to extreme pain.
“She was starting to go inward and having a much harder time in her body,” Colombatto said. “She said, ‘I’m done with this, I just want to be done.’ And I’d say, ‘You can’t be done until you’re done.’ That was lighthearted and fun, but I also think it shocked her.”
She added: “There was a point with the pancreatic cancer where it’s winning. Pancreatic wins. That was the hardest-working death I had ever seen. She was working at getting out of her body.”
At 12:40 a.m. on Dec. 1, her work was over.
Was it a good death?
“She was showing us what death without fear looks like,” said Catharine DeLong, a music thanatologist who had played the harp for Weisberger over Zoom from Salt Lake City but arrived in New York too late to play by her bedside.
It was not the death Weisberger wanted — without drugs, expiring peacefully with her friends around her, sharing her last thoughts. The final epiphany, in those last hours, was how painful her death was, how essential drugs really were.
The revelation of the weeks before her death was more significant, said Emily Eliot Miller, an end-of-life doula who often argued with Weisberger about her abstract fixation on a “good death.”
“I think Shatzi knew that what she needed most was love and witness,” Miller said. In that sense, Miller said, Weisberger succeeded. “She had the death she wanted: full of love, meaningful goodbyes and media attention.”
As her body, bathed and oiled by her close friends, left the apartment around 5 a.m. on Dec. 1, Colombatto chose the exit music. At full volume, she blasted Frank Sinatra’s “My Way.”


More Stories
Southwest’s epic holiday meltdown could cost it $825 million
From orphans to best friends, Woodland Park Zoo welcomes new bear cubs
Tacoma zoo welcomes new Sumatran tiger